Skin Cancer Treatment
The Auckland Plastic Surgical Centre specialises in the surgical treatment of skin lesions. We utilise careful analysis, diagnostic accuracy and technical expertise in removal and reconstruction to leave the least noticeable scars.
Early diagnosis is vital, and this will often be done through biopsy (removal of some or all of a lesion for microscopic analysis and laboratory identification). For small lesions, this may also involve treatment by complete removal (an excisional biopsy). For more extensive lesions, a small piece of affected tissue is analysed (a punch or incisional biopsy) and if the diagnosis calls for it, we make a removal and reconstruction plan. Most biopsies and tumour excisions and repairs are done under local anaesthetic and, depending on your policy, are usually covered by medical insurance.

Malignant Skin Conditions
With the exception of malignant melanoma, these do not usually spread to other parts of the body (metastasize) and are not usually life-threatening, unless ignored for a prolonged time. Smaller lesions can be simply removed and sutured, while larger lesions may be removed and closed with a suitable local tissue flap or graft.
What to look out for: Any lesion that turns black, is growing, ulcerates, or alternates between healing over and crusting/scabbing. These need to be thoroughly checked under good lighting by an expert, and a biopsy taken if there is any doubt about the diagnosis. If a lesion is being treated, yet continues to grow or spread, please seek a second opinion from a Plastic Surgeon or Dermatologist. As with any form of cancer, early diagnosis and treatment are vital. In addition, the smaller the skin lesion when diagnosed, the smaller any resulting scar will be. Factors such as chronic/ long-term sun exposure, genetics, immunosuppression, childhood sunburns, and occupational hazards such as exposure to certain chemicals, can increase the risk of developing skin cancer. Likewise, previous injuries such as burn scars have an increased tendency to develop into an SCC (Squamous Cell Carcinoma).
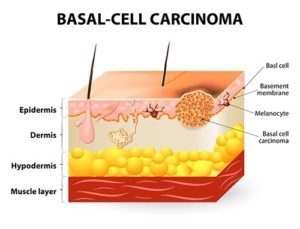
Basal Cell Carcinomas (BCCs)
Many forms of Basal Cell Carcinoma (BCC) ” the commonest skin cancer ” develop in direct relationship to sun exposure. We treat many patients with BCCs ” particularly those with fair or red hair, who freckle and burn easily, and whose work or lifestyle involves significant exposure to sunlight. More than 80% of BCCs occur in areas directly exposed to sunlight, including the head and neck.
What to look out for: Slow growing, BCCs very rarely metastasize but are usually locally invasive and destructive. They form in the basal layer of cells in the epidermis, and their appearances can vary widely.
While simple surgical removal is often the best way of treating most of these lesions, other options such as cryotherapy (freezing with liquid nitrogen), curettage, electrodesiccation and x-ray irradiation have proved effective. Recent advances have shown that photodynamic therapy may be useful for other forms of BCC.
Squamous Cell Carcinomas (SCCs)
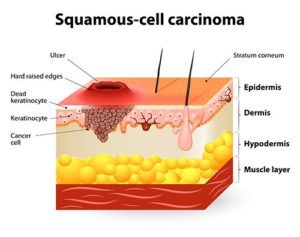
SCCs range from superficial to deeply invasive. The more superficial form ” SCC in situ ” has abnormal cells in the skin’s upper layer, without affecting the deeper layer. There are several variations of this SCC, including Bowen’s disease, which may occur anywhere on the body, with some specific forms affecting the genitals (unrelated to sun exposure). Treatment involves simple diagnosis and removal.
What to look out for: More invasive forms of SCC are common. They often produce excessive keratin (white, flaky dry skin) and have indistinct margins. They almost always occur in very sun-damaged skin with other signs of chronic UV radiation. Around 40% arise from pre-existing actinic keratoses (thick, scaly, or crusty patches of skin) and about 3-5% have the potential to metastasize, although SCCs on the lip have a 10-30% risk of metastasizing. Old scars such as burns or chronic ulcerations make the development of an SCC and metastasis more likely.
Early diagnosis by biopsy is key. We can treat the SCC with removal and reconstruction.
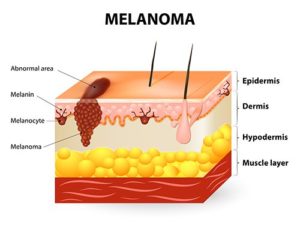
Malignant Melanoma
This, the most serious skin cancer can and does spread, sometimes rapidly and unpredictably, to other parts of the body. Caught early, skin cancer can usually be treated simply and quickly by excision. But if malignant melanoma is left untreated or detected late, it is often fatal.
There are several different types of melanoma, identified by their growth pattern. The most benign is intraepidermal malignant melanoma in situ, which does not metastasize and is curable if completely removed. Left alone, this will begin to grow beneath the skin. Its depth and thickness correspond to the rate of metastasis and survivability. Understanding this growth pattern helps account for the clinical variants of malignant melanoma encountered.
Superficial Spreading ” (about 60% of all melanomas spread outwards as a flat, irregular area of pigmentation with occasional nodules)
Nodular Melanoma: Rapid and uniform vertical growth creating a nodule or lump
Lentigo Maligna: The malignant degeneration of a flat, evenly pigmented patch, almost always seen on the face. Initially, there may be dark speckling on a pigmented background and later vertical growth may create a nodule.
Acral Lentiginous Melanomas: These are rare but occur on the genitalia, palms, the soles of the feet, and under the nails. Any pigment under the nail should be examined and differentiated from a blood stain under the nail, commonly seen after trauma.
Spotting a malignant melanoma is not quite as easy as ABC but this mnemonic may help:
A = Area, has there been a change in size, suggesting that the lesion has grown, or Asymmetry since a malignant lesion is likely to be asymmetric;
B = Border irregularity;
C = Colour variegation (shades of red, blue, black and brown may be visible);
D = Diameter typically greater than 6mm;
E = Everything Else, including itching, bleeding, ulceration or feeling constantly aware of it.
Treatment usually involves removal as a biopsy for diagnosis. Depending on the diagnosis, a removal of some surrounding tissue may also be needed, plus other surgical measures. These details will be discussed with each patient on a case-by-case basis.
Keratoacanthoma: These lesions can look very dramatic, growing rapidly over a few weeks or months. They usually grow singly in sun-damaged areas and look like a volcano: a flesh-coloured nodule with a central crater filled with keratin. Although possibly benign and self-healing, they may look like squamous cell cancers, and are usually best treated by immediate removal and reconstruction.